You’ve been diagnosed with Mesothelioma. Now What?
Surgery?
Chemotherapy?
Radiation?
Immunotherapy?
Is Surgery Advisable? Who decides whether it’s “Resectable?”
You’ve been diagnosed with Mesothelioma. Now What?
Is Surgery Advisable? Who decides whether it’s “Resectable?”
Most pleural mesotheliomas are potentially operable. The clinical term for that is “resectable.” Many factors influence the resectability of the mesothelioma. Variables include the cell type (epithelial vs sarcomatoid vs biphasic), lymph node involvement, the fitness of the patient, and whether the tumors have spread to other organs, such as the lung itself.
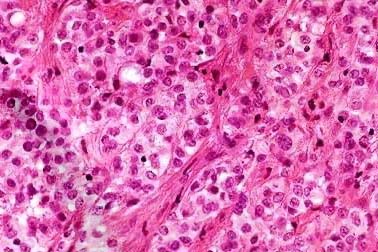
Epithelial cell type
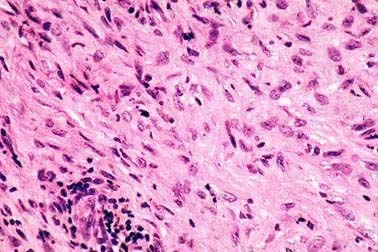
Sarcomatous cell type

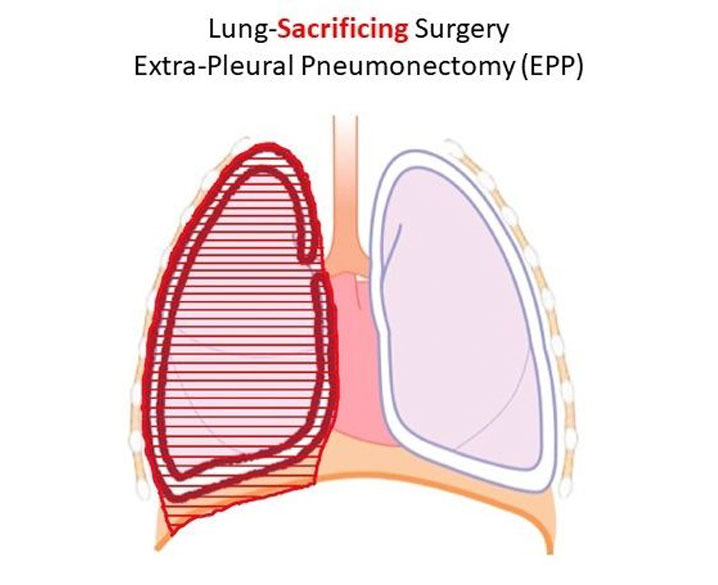
Another big variable is this: Who decides? Mesothelioma is a rare and difficult disease to both diagnose and treat. Few doctors, even surgeons, have the experience to credibly make the call whether the tumor is “resectable.” There’s a debate between thoracic surgeons on whether mesothelioma is resectable. For decades now the only surgery thought to be helpful was a complete removal of the lung inside the tumor, aka, “extra-pleural pneumonectomy” (the EPP).
A small but growing group of surgeons, led by Dr. Robert Cameron at UCLA Medical, has shown the best surgery is the “pleurectomy/decortication,” or P/D, a procedure in which the surgeon must meticulously remove the tumor from the ribcage, diaphragm and lung itself. The EPP takes about 2.5 hours. The P/D takes around 10 hours. So, you can see why many surgeons shy away from the P/D.
Nationwide, there are many more oncologists than thoracic surgeons. For decades, most experts have agreed that surgery with radiation offers a greater chance for longer survival than chemotherapy alone (such as Alimta-Cisplatin). Now we’re seeing ads on television touting Opdivo/Yervoy as an immunotherapy option. We applaud the pursuit by drug companies to find meaningful treatments for meso patients. However, there is no data to suggest that Alimta-Cis or Opdivo/Yervoy offer meso patients a better chance of longer survival than any multi-modal approach that includes surgery at its foundation.
It’s well known that surgeons will prefer surgery, and oncologists will prefer chemotherapy or immunotherapy. They prefer what they know. So, should you automatically trust the judgment of an oncologist who has just advised you that your tumor is NOT resectable? That your best option is to hook up to the last cocktail of chemotherapy or immunotherapy drugs that are in fashion?
We don’t think so. Would you trust a bone doctor to tell you whether your heart disease needs surgery? What treatment course to pursue is both the first and most important decision you will make. You should make sure you get an opinion on the resectability of your meso tumor by a thoracic surgery with years of experience in actually removing meso tumors from the human chest.

The purpose of surgery is to remove all visible tumors, thereby relieving pressure which the growing tumor places on the internal organs and preventing the tumor from spreading to other parts of the body. Removing tumor bulk can also offer pain relief, as a growing tumor will compress against the lung, ribcage, heart and nerves.
As mentioned above, there are two surgical procedures which are used for treating mesothelioma: the Extrapleural Pneumonectomy (EPP) and the Pleurectomy /Decortication (P/D).
Surgery is the foundation of a successful multi-modal treatment plan. See the video above to better understand the typical progression of mesothelioma. The first question to ask: Is the tumor operable? Only an experienced thoracic surgeon can credibly answer that questions.
The EPP, is a radical procedure where the surgeon removes the lung on the side of the mesothelioma cancer along with the pleura lining the chest wall on that side, the diaphragm (thin breathing muscle) on that side, maybe the pericardium (the sac around the heart), and any nearby lymph nodes. The diaphragm and the pericardium are then rebuilt with man-made materials.
Because of the radical nature of this procedure, and the fact that the patient will be left post-operatively with only one lung, it can only be performed on patients who meet certain criteria such as good cardiac and pulmonary functioning.
The P/D, is a less radical procedure in which all of the pleura lining the chest wall (on the side with the mesothelioma cancer) is removed, along with the pleura coating the lung on that same side. The pleura coating the mediastinum and the diaphragm is also removed. The lung and diaphragm muscle are not removed.
The type of surgery also depends on the hospital and surgeon’s experience along with the details of each patient’s cancer and overall health.
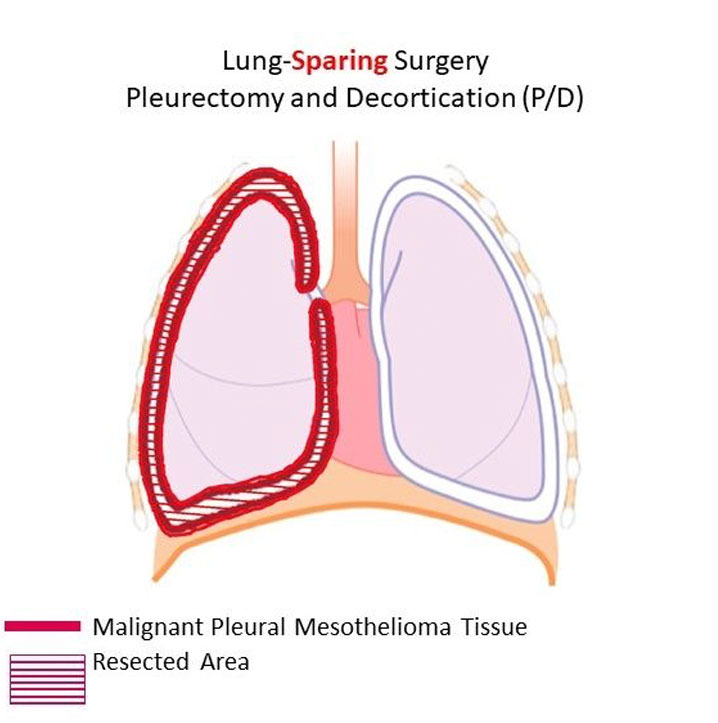
Medical studies continue to suggest that the P/D is the preferred surgery because there are fewer problems linked to it versus the EPP, and the overall outcomes are much the same as, if not better than EPP.
You can view several studies from mesothelioma cardiothoracic surgeons comparing the EPP and P/D.

Dr. Robert Cameron is the Chief of Thoracic Surgery at the West Los Angeles VA Medical Center.
Dr. Cameron is also a Professor of Clinical Surgery, Cardiothoracic Surgery and Surgical Oncology at the University of California in Los Angeles, California and the head of the Comprehensive Mesothelioma Program at UCLA Medical Center and serves as the Scientific Advisor of the Pacific Mesothelioma Center.
Dr. Cameron has been treating mesothelioma patients for over 25 years. He is the innovator of the lung-sparing P/D surgical procedure and has performed the procedure on over 300 patients to date.
Dr. Cameron’s approach to treating mesothelioma has always been to “Remove the tumor, save the lung and treat the disease as a chronic illness.”
In Summary, before accepting your doctor’s opinion that you are not a surgical candidate, before agreeing to pursue chemotherapy, or immunotherapy, please consider asking Dr. Cameron for his opinion. He will give the unbiased, unvarnished truth.
Phone: 310-267-4612
Email: RCameron@mednet.ucla.edu
It makes no sense from an oncology standpoint, because a surgeon cannot rid a mesothelioma patient of every last cancer cell and cure them that won’t happen. Once you accept that, then you can understand why P/D is the best surgical option with the least side effects, the least chance of dying and a better chance of getting as much tumor clearance as possible.”
-Dr. Robert Cameron, 2020


At Worthington & Caron, PC, our motto is “Asbestos Lawyers for Life.” The meaning is twofold – we are 100% committed getting asbestos cancer patients the justice they deserve and the life-extending medical treatment they need.
Since 1989, Worthington & Caron has been representing asbestos cancer patients and generated over 2.5 billion dollars in settlements and verdicts, including:
In addition, Worthington & Caron’s overwhelming commitment to mesothelioma research sets us apart from other lawyers. We have donated to this cause more than any other law firm we are aware of.
If you or someone you care about has been diagnosed with asbestos-related cancer or mesothelioma, please contact us.